One of my clients – a mid 50’s male who lives an active lifestyle, had been living in the Netherlands & recently moved back to the US – contacted me complaining of heel pain on his left foot, he referred to it as plantar fasciitis.
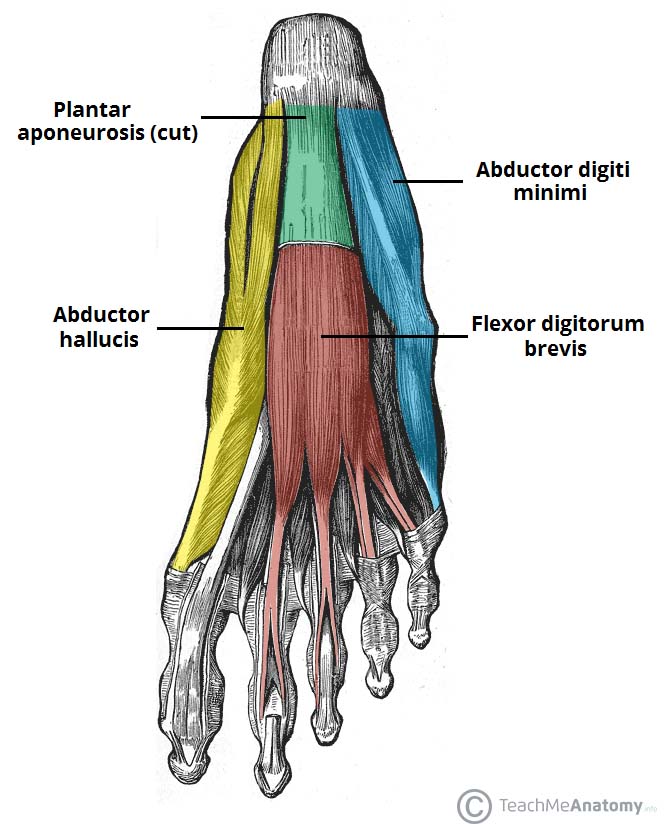
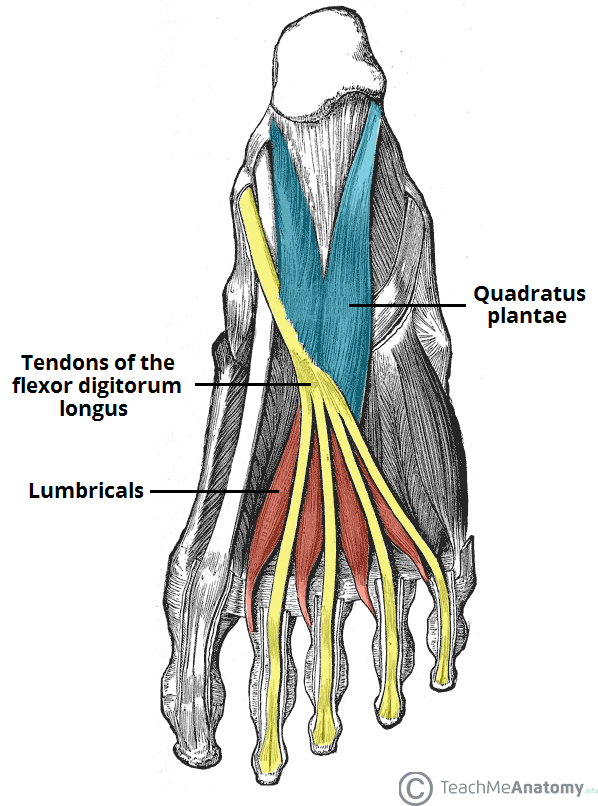
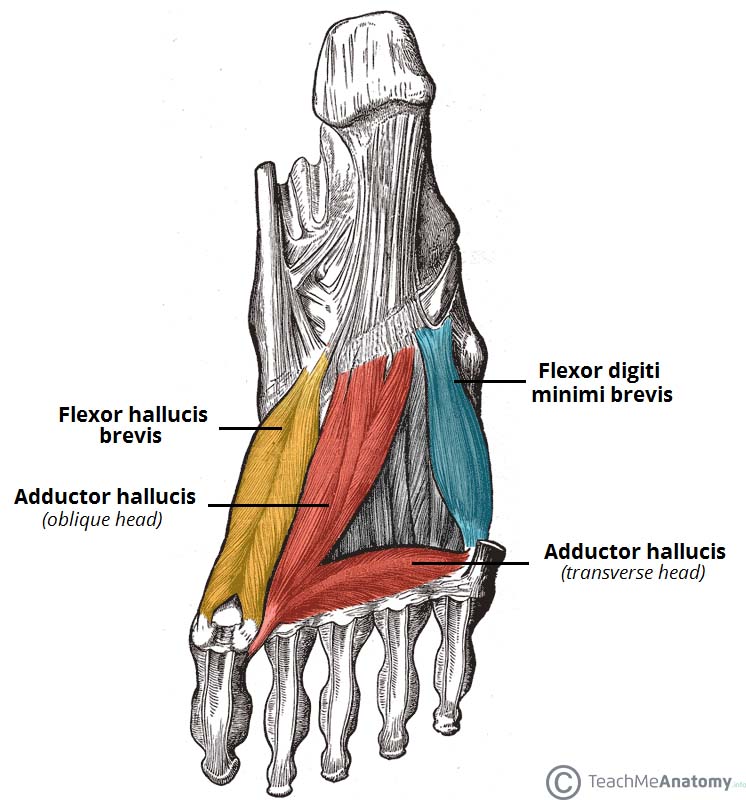
For reference, here are the plantar (bottom of the foot) layers of your foot muscles:
He came in a week later for an initial evaluation of this heel pain. We discussed what was going on with the heel (it wasn’t plantar fasciitis), how he was doing overall, and I performed a manual diagnostic exam. I then laid out my informed diagnosis and full treatment plan.
I haven’t seen him since….why not? Well, he hasn’t had pain since, nearly 5 months!
1 visit, problem solved.
It’s not too good to be true. That’s the power of a detailed diagnosis combined with addressing multiple systemic and holistic factors. Keep reading for the full details.
I. The context of his heel pain
As per our conversation:
- the heel pain began approximately 5 months prior
- the pain is on the medial (inner), proximal aspect of his heel
- the heel pain gets worse the longer he’s on his feet
- the heel pain is worse when he’s barefoot (he loves to be barefoot)
- tried different shoes, treatments – nothing seems to work
- recently took up a new job with lots of added stress
- recently has had trouble sleeping
- dealing with a new lifestyle and culture, having just moved back to the States
II. Manual diagnostic (heel pain & rib cage)
I’ll spare you the complete diagnostic details but here are the tissue & musculoskeletal issues I found (all on his involved, left, side):
- Left leg
- Posterior tibial (post-tib) weakness
- Calf weakness
- Hip abductor weakness
- Gluteus maximus (glute max) weakness
- Over-use of the flexor hallucis brevis (FHB)
- Moderate tenderness to palpation
- Medial aspect of the calcaneal fat pad
- Flexor digitorum brevis
- Rib cage
- Rotated to the right
III. The Total Picture & Assessment
The affected tissue and musculoskeletal factors are part of the equation but I don’t treat in isolation. I always take the full holistic picture – humans are robust and complex systems after all.
Based on our conversation and manual diagnostic exam, I came up with the following assessment:
There were two micro (local) factors , four mezzo (systemic) factors, and one overlying macro (contextual) factor all contributing to his heel pain.
A. Micro factors
- Tissue
- Irritated calcaneal fat pad
- Irritated flexor digitorum brevis muscle
B. Mezzo factors
- Bio-mechanical
- Weak posterior tibialis and weak hip abductors were likely biasing him into prolonged pronation
- Weak posterior tibialis, calf and glute max were increasing the amount of force into his heel
- Rotated rib cage was altering his diaphragm’s movement
- Breathing
- Difficulty with deep exhalation and holding exhalation
- Neuro-cognitive
- He was in pain for multiple months. When the brain begins to anticipate pain, your system becomes more sensitized to pain and begins to view previously innocuous movements as threatening. This generates a pain response & more sensitivity. It’s a vicious cycle.
- Gastro-intestinal (GI)
- He was experiencing stomach and digestion irritation for months – possibly due to re-acclimating to a US diet after being in the Netherlands for years. Irritation of the GI system can create systemic inflammation.
C. Macro factors
- High stress
- New role at work with significantly increased responsibility
- Re-acclimating to a new environment
- Much longer commute with more traffic than he was used to
- Trouble sleeping
IV. How we solved the heel pain
A. In clinic manual treatment
- 20 minutes of manual treatment to his FDB and heel pad
- 10 minutes of rib cage facilitation to improve rib cage positioning during breathing
B. Education
- The connection between the brain, body, and pain
- How stress affects the body and pain
- Book recommendations
C. Targeted activity
- Foot intrinsic muscle strengthening
- Complete 20 reps
- Posterior tibial strengthening progression
- Work up to 30 reps. Once you can complete 30 reps, move onto the next part of the progression.
- Calf strengthening
- Hip abductor strengthening
- Gluteus maximus (glute max) strengthening progression
- Work up to 15 reps. Once you can complete 15 reps with good form, move onto the next part of the progression.
I normally only give 1-2 activities to start but he was extremely motivated, wanted the full arsenal, and I was confident he wouldn’t be overwhelmed by the amount of information.
D. Motor patterning
- Decreasing over-use of his flexor digitorum brevis and longus (FBD and FDL)
- Improving his breathing pattern (exhale-pause breathing technique)
E. Stress
-
Left nostril breathing
- Breathing meditation
- 20/80 analysis
- AM routine
- Sleep strategies
F. Nutrition
-
Referral to a trusted integrated & functional medicine dietician – Kim Kelly MS RD, at Functional Healing
E. External device
-
I recommended that he purchase a heel cup insert to use in the short-term to help with with the heel pad irritation
V. The Result (1 visit, heel pain free)
My client was committed to the plan, we constantly stayed in contact, and he’s been heel pain free for 5 months after only 1 in-person visit. Further, he now has the tools and knowledge to take full ownership & help himself if this problem arises again.
We continue to have a strong working relationship so if he ever has questions or concerns, or if he simply wants to grab lunch & catch-up, he can always contact me directly.
A great outcome that is a product of the plan, process, and dedication to it.
Are you having heel pain of your own or just fed up with aches, pains, injury, or stress? Click the button below to book a free 15 min phone consult with our Doctor of Physical Therapy to discuss your questions/issues and setup a free injury screening. Together, we’ll create a plan to reduce pain, prevent future injury, and surpass your goals.
